Modern medicine has made it possible for seniors to live longer, healthier lives. Yet, longevity often comes with complexity: multiple chronic illnesses requiring multiple medications. This phenomenon—known as polypharmacy—is both a reflection of medical progress and a growing clinical challenge.
While these medications control hypertension, diabetes, or heart disease, they also expose patients to increased risks of drug–drug interactions, cumulative toxicity, and organ stress. For physicians, the key to safe prescribing is not merely pharmacologic knowledge but continuous laboratory monitoring.
Routine testing can reveal subtle biochemical changes before symptoms arise, allowing timely intervention. For elderly patients, these small insights can make the difference between stability and avoidable hospitalization.
The Growing Concern of Polypharmacy
Polypharmacy, typically defined as the use of five or more concurrent medications, has become common in geriatric care. According to international studies, nearly 40–50% of adults over 65 fall into this category.
While often unavoidable, polypharmacy increases the risk of adverse drug reactions (ADRs), which account for up to 10% of hospital admissions among the elderly. Age-related changes—slower metabolism, reduced renal clearance, and altered body composition—magnify the effects of even standard drug doses.
Drugs that once performed safely in midlife can suddenly cause liver stress, electrolyte imbalance, or renal dysfunction in later years. Regular laboratory testing is therefore not optional; it is the foundation of safe pharmacologic management.
AsiaLabs: Keeping Precision Testing In-House
AsiaLabs helps clinics keep essential geriatric testing in-house, combining speed with clinical precision. For elderly patients on chronic medications—such as antihypertensives, NSAIDs, or statins—routine monitoring is not optional; it’s preventive medicine. AsiaLabs recommends a structured approach that includes:
-
Liver Panel (ALT, AST, GGT, BIL T, BIL D) – to detect early signs of hepatotoxicity before symptoms appear.
-
Renal Function (Creatinine, eGFR, Urea) – essential for diabetics and those on ACE inhibitors or nephrotoxic agents.
-
Electrolytes (Na⁺, K⁺, Cl⁻, Ca²⁺) – to identify imbalances linked to diuretics or multiple concurrent medications.
All of these tests are processed with ISO 15189-certified accuracy and a two-hour turnaround time, allowing physicians to act on reliable data the same day. They can also be bundled for cost-efficiency, making comprehensive monitoring accessible to every clinic.
With AsiaLabs, you don’t just manage disease—you prevent complications before they happen. Each result contributes to a safer, closed-loop model of elderly care, where diagnostics, decision-making, and follow-up remain connected under one roof.
Panel 1: Liver Function Tests (LFT) — The Metabolic Gatekeeper

The liver is the body’s central biochemical engine. It metabolizes nearly 70% of prescription drugs, including statins, antibiotics, psychotropics, and antiepileptics. With aging, hepatic blood flow and enzyme activity decline, reducing clearance rates.
When multiple drugs converge on this system, silent hepatic stress becomes a real risk. Monitoring ALT (alanine aminotransferase), AST (aspartate aminotransferase), ALP (alkaline phosphatase), GGT (gamma-glutamyl transferase), total bilirubin, and albumin can detect early liver strain long before clinical symptoms appear.
Clinical insight:
Even mild enzyme elevations—1.5 to 2 times the upper reference limit—should not be ignored in elderly patients. These may signal the onset of hepatocellular injury. Drugs such as amiodarone, methotrexate, valproate, and certain antifungals are particularly notorious for inducing slow, cumulative toxicity.
Regular LFT monitoring allows clinicians to adjust dosages or switch regimens before irreversible liver damage occurs. In AsiaLabs’ workflow, liver panels are batched with metabolic tests, providing same-day results to support swift clinical decisions.
Panel 2: Renal Function Tests — The Excretion Watchdog
If the liver is the metabolic gatekeeper, the kidneys are the body’s filtration system—and polypharmacy puts them under constant strain.
Drugs such as NSAIDs, ACE inhibitors, diuretics, and aminoglycosides can impair renal perfusion or tubular function. In the elderly, glomerular filtration rate (GFR) naturally declines with age, making kidneys less resilient to additional stress.
Monitoring serum creatinine and estimated GFR (eGFR) is the first step in assessing kidney performance. Yet, a more complete view includes blood urea nitrogen (BUN), electrolyte levels (Na⁺, K⁺, Cl⁻), and urine albumin/creatinine ratio.
These indicators together help identify both functional decline and early microvascular damage.
Clinical best practice:
-
Establish a baseline renal profile before initiating any nephrotoxic drug.
-
Recheck within two weeks after starting or changing such medications.
-
Maintain quarterly reviews for chronic users, especially diabetics and hypertensives.
Detecting early kidney impairment prevents cascading complications—drug accumulation, fluid imbalance, or electrolyte disturbances—that can otherwise lead to hospitalization.
AsiaLabs’ renal panels are processed under ISO 15189-accredited protocols, ensuring analytical precision that clinicians can rely on when fine-tuning medication doses for frail patients.
Panel 3: Electrolyte and Metabolic Panels — The Balance Sheet
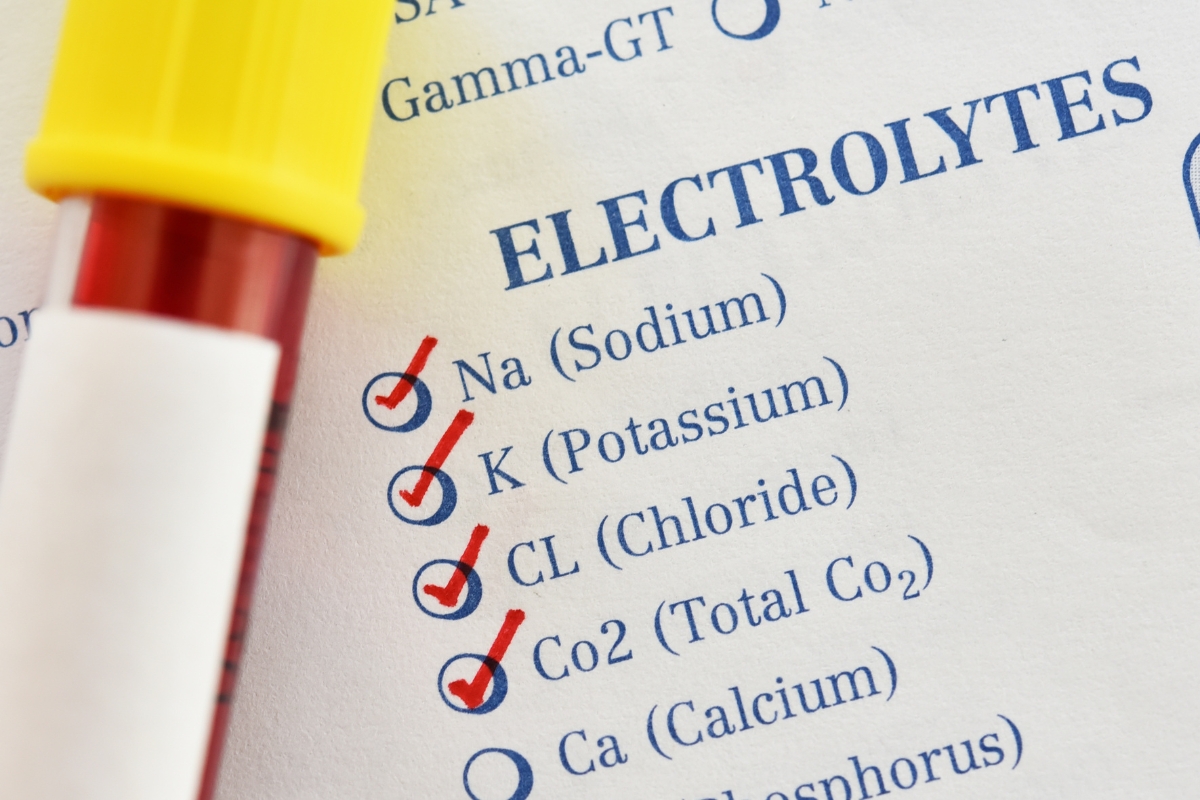
Homeostasis is fragile in aging bodies. Many medications—including diuretics, digoxin, proton-pump inhibitors, and SSRIs—can disrupt electrolyte balance, leading to serious consequences.
Even small deviations in sodium, potassium, calcium, magnesium, or chloride can trigger arrhythmias, muscle weakness, confusion, or falls—events often mistaken for “normal aging.”
Routine electrolyte screening identifies imbalances early, allowing clinicians to modify therapy before symptoms manifest.
Equally important are metabolic markers such as fasting glucose, HbA1c, and lipid profile, which reveal side effects from corticosteroids, beta-blockers, or antipsychotics.
These values not only safeguard against drug toxicity but also enable integrated care for comorbid conditions like diabetes and dyslipidemia.
Clinical insight:
-
Always correlate potassium trends with medications like ACE inhibitors or diuretics.
-
Watch for sodium shifts in patients on SSRIs or carbamazepine.
-
Monitor calcium and magnesium when using proton-pump inhibitors long term.
Electrolyte and metabolic panels thus serve as a vital safety net in the complex pharmacologic landscape of geriatric care.
Clinical Integration: One Draw, Multiple Insights
The traditional model of ordering separate tests for each system is inefficient and burdensome for older patients. Modern laboratories like AsiaLabs integrate all three essential panels into a single venipuncture session, minimizing discomfort and maximizing data yield.
Once collected, samples are processed through automated analyzers, ensuring consistent calibration across liver, renal, and electrolyte assays. Results are delivered digitally within 24 hours, allowing physicians to review organ tolerance, drug efficacy, and metabolic stability in one snapshot.
This integrated approach transforms routine monitoring from a fragmented process into a comprehensive safety audit. Physicians can quickly correlate trends—rising liver enzymes with stable creatinine, or electrolyte shifts following a new prescription—and adjust management accordingly.
For elderly patients who may struggle with mobility or venous access, reducing repeated draws is not just efficient—it’s compassionate care.
Moving Toward Proactive Geriatric Monitoring
Reactive medicine—waiting for symptoms to appear—is no longer acceptable in an era where laboratory data can predict problems early. For seniors on complex drug regimens, scheduled testing is preventive medicine in its purest form.
Regular panels allow clinicians to:
-
Detect subclinical toxicity before it progresses.
-
Optimize dosing based on organ function trends.
-
Avoid unnecessary hospital visits through early outpatient interventions.
-
Enhance patient confidence by demonstrating proactive oversight.
At AsiaLabs, we advocate for structured geriatric monitoring schedules:
-
Baseline testing before initiating any long-term therapy.
-
Follow-up panels within the first month of medication changes.
-
Quarterly reviews for ongoing therapy involving hepatotoxic or nephrotoxic agents.
Each result is digitally archived and trend-analyzed, allowing clinicians to view long-term trajectories—an invaluable tool for managing chronic diseases like hypertension, diabetes, and heart failure.
Conclusion
For elderly patients, every pill offers promise—but also potential peril. The cumulative effects of polypharmacy can quietly erode organ health, often without visible warning signs. Routine laboratory monitoring is the physician’s most powerful defense against these risks.
By consistently assessing liver, renal, and electrolyte panels, clinicians can ensure that treatment remains effective, safe, and personalized.
What seems like a simple blood draw becomes, in truth, a vital checkpoint for quality of life.
At AsiaLabs, our mission is to make this level of monitoring accessible to every clinic and every senior. Through digital connectivity, same-day turnaround, and ISO-accredited accuracy, we help healthcare providers protect their most vulnerable patients—those who rely on medicine every day to live well, age safely, and stay independent.